Voices of U of U Health
“Meet Me Where I Am”
After nearly 30 years of abuse, addiction, incarceration, homelessness, and serious health issues, Adolphus Nickleberry decided it was time to seek help. His moving story is the subject of “Meet Me Where I Am,” a documentary short film produced by University of Utah Health that debuted during Sundance Film Festival 2022.
U of U Health is proud to be the official health and wellness sponsor of Sundance for six years running. In keeping with the festival spirit, we embrace the opportunity to enrich the community by amplifying new voices and models of care through the ongoing series “New Narratives in Health.” With generous support from the Kahlert Foundation, award-winning filmmakers Ross Kauffman, André Robert Lee, and Robin Honan show how Nickleberry combatted the underlying traumas of his childhood—with the assistance of the Intensive Outpatient Clinic, a unique program at U of U Health—to begin a new chapter in his life.
The film debut was paired with a panel discussion featuring Nickleberry, his dedicated health care team, and the talented production team.
Helping Those Who Need It Most
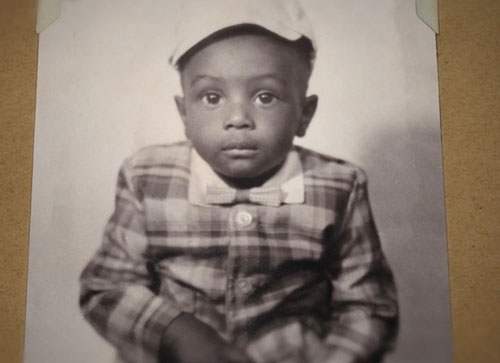
“I was tired of feeling so bad, so alone. I wanted to feel safe and cared for,” explained 61-year-old Nickleberry. “I wanted to see my daughter and grandkids again. And the people at the Intensive Outpatient Clinic seemed serious about helping me get my life back.”
“When I was approached about doing the film, I was pretty skeptical,” Nickleberry added. “I was used to going out and getting high to avoid stuff, but now I was being asked to open up and tell my story.”
His story paints a vivid picture of those in our communities who have been put at increased risk of poor health outcomes. University of Health Plans and the Intensive Outpatient Clinic (IOC) saw an opportunity to provide medically and behaviorally complex Medicaid members with individualized treatment plans while creating efficiencies for the health system. These patients make frequent visits to the ER and are often hospitalized for prolonged periods of time. Frequent touch points with an integrated care team can often reduce both those metrics.
In 2017, “We took a risk to fund the IOC,” explained Chad Westover, CEO at U of U Health Plans. “We looked at it and realized there were savings to be had and lives to be saved. It just made sense for U of U Health Plans to take a chance on it.”
Ultimately, it’s not about making money, it’s about saving money. This model of care is a great way to save money and help those who need it most.
Individualized Treatment
Like Nickleberry, this population of individuals typically has a significant trauma history. Most ERs and health centers are not equipped to provide the more intensive medical and behavioral health support these patients need for an extended period of time.
The IOC provides a unique model of treatment. We help identify patients who frequent our emergency department, seeking help for a myriad of medical and mental health needs. By taking them under our wing, we alleviate the huge amount of time, cost, and burden on hospital and health center teams.

IOC patients receive a treatment plan and support specifically designed around their needs. Establishing trust and a good provider-patient relationship takes time. The clinic offers the right medical providers, therapists, and ancillary staff to meet the complex needs of its patients.
I know when I go in to meet with a patient, I can really find out how they are doing and feeling. I have the time I need to spend with patients. It’s a luxury most doctors don’t have. Because our staff is small, we also keep our patient base small, so we are able to continue providing personalized, intensive care.
This high-touch, personalized approach to patient care can be challenging at times. The IOC staff makes a special effort to take care of one another just as they take care of their patients. “I can’t imagine working anywhere else,” said Christina Cackler, LCSW, behavioral team lead at IOC. “Although my job can be extremely stressful, it is also extremely rewarding. I love what I do!”
