Voices of U of U Health
Overcoming Bias in Medical Education
Taking steps to create a learning environment free of bias took center stage at last month’s School of Medicine Core Educator Retreat. It is a goal and expectation of our curriculum, and our faculty, to approach everything we do with as little bias as possible.
We are fortunate to have a community of core educators who are willing to take risks, have open and honest conversations, and make continuous improvement.
Faculty Driven, Learner Focused

As the School of Medicine continues to implement recommendations from the Anti-Racism Commission, fostering justice, equity, diversity, and inclusion within our program is a top priority. In addition to diversifying our medical school class, this work includes creating psychologically safe spaces where students can learn from their mistakes while faculty and learners can give each other honest, constructive feedback.
Faculty focus groups provided input on content and structure for the core educator retreat. These groups expressed an interest in practical steps for mitigating bias and systemic racism in our clinical and learning environments. With that in mind, the retreat aimed to provide faculty with greater awareness of our own implicit biases, and their impact on us, our learners, and our patients. Methods and tools were introduced to help everyone have the best possible experiences in our teaching and learning.
With an emphasis on developing better educational materials, interactive breakout sessions explored best practices for:
- Writing clinical cases without reinforcing stereotypes about patients.
- Avoiding bias and stereotyping in student assessments.
- Crafting learner evaluations that emphasize skills rather than personal characteristics.
Room to Improve
The core educator retreat was an opportunity to acknowledge critical areas of our program that need to change and commit to a different, better path moving forward. Attendees reviewed AAMC Year Two survey data and graduation questionnaire data from 2016-2020. Both surveys compare how University of Utah medical students rate aspects of their medical school experience relative to other medical students nationwide.
Survey data indicates U medical students did not feel prepared to care for diverse patients. Overall, they rated their equity, diversity, and inclusion experience below the 10th percentile nationally.
When it comes to mistreatment, survey data shows our graduating students experience more mistreatment than students at other schools—falling below the national average. Historically, our female students have experienced more mistreatment than male students. And BIPOC students have experienced mistreatment more often than white students.
This data has been shared with the School of Medicine Executive Committee and all academic department chairs. Departments are charged with elevating awareness and developing action plans to address mistreatment. As we continue taking steps to foster an inclusive, anti-racist culture, we can turn the tide on these concerning trends.
Cultural Humility
Included in the School of Medicine Anti-Racism Commission report is the recommendation to “allow students to give course directors and presenters feedback regarding their cultural humility.” The School of Medicine Curriculum Committee is implementing this in the following ways:
- Define cultural humility to facilitate a shared understanding.
- Develop a rubric by which cultural humility can be evaluated using agreed-upon criteria.
- Train faculty on the rubric specifically and cultural humility in general (starting with January 2022 Core Educator Retreat).
- Train select students to assess a sample of faculty and sessions with the rubric.
- Eventually train all students over two years.
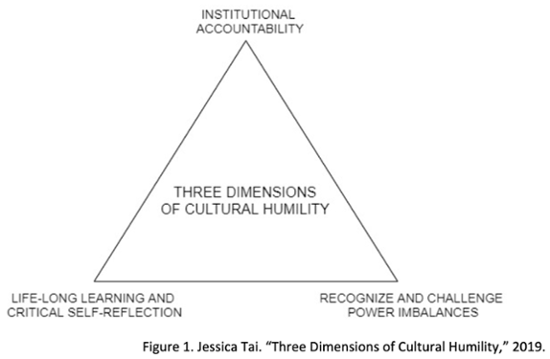
We intentionally selected a developmental rubric designed to facilitate growth. It should be flexible enough that students can use it to assess faculty and faculty can use it for self-assessment, to assess each other, and to evaluate our curriculum.
In breakout groups, core educators were asked to evaluate a sample lecture presentation using the new rubric. We challenged each other to think about the content we choose to use in our instruction and the effect it can have on those participating in the curriculum. Faculty provided helpful feedback for developing this rubric further. We’re optimistic that adopting this tool into our culture and using it regularly can help us sustain long-term results on our path of improvement.
Changing for the Better, Together
More than 60 School of Medicine faculty, ranging from basic science to those on the clinical frontline, participated in the core educator retreat. Our work to mitigate various forms of bias and racism aligns with the ongoing transformation of our medical education program. Thanks to the proactive leadership of core educators and other collaborators, we have a clearer understanding of where we are today. In partnership with our students, we are committed to doing and becoming better in the future.




