Author: Doug Dollemore
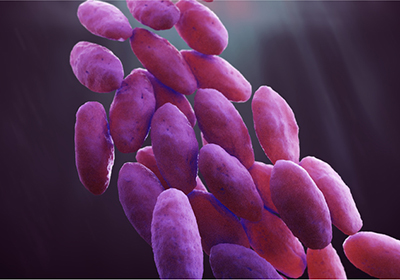
Eradicating antibiotic-resistant bacteria in asymptomatic people before they can spread these microbes to others could be far more cost-effective than treating hard-to-eradicate infections once they occur, according to University of Utah Health researchers. Photo credit: Getty Images
Each year, more than 2.8 million antibiotic-resistant infections occur in the United States, according to the Centers for Disease Control and Prevention. More than 35,000 Americans die of these infections annually, and the cost is staggering, accounting for more than $2 billion in added health care expenditures nationwide in 2018.
But suppose a different approach to treatment and prevention could lead to reduced costs and fewer patients getting these types of infections with better outcomes? Well, a new study suggests that scenario isn’t out of reach.
Using computer models, University of Utah Health scientists found that detecting and eliminating antibiotic-resistant bacteria in asymptomatic people before they can spread these microbes to others could be far more cost-effective than treating hard-to-eradicate infections once they occur.
“Individuals who are carriers of antibiotic-resistant bacteria but aren’t actually sick may receive some direct benefits from this approach,” says Richard E. Nelson, PhD, a co-author of the study and a research associate professor in the Division of Epidemiology at U of U Health. “However, what really matters is that removing or decolonizing the bacteria from their bodies could also prevent them from transmitting the disease to others who may be susceptible. This indirect benefit is huge in terms of reducing medical costs and extending life.”
The study appears in a special issue of Clinical Infectious Diseases that features research from several U of U Health scientists.
The researchers developed a mathematical transmission model to test the effects of two hypothetical antibiotics on carbapenem-resistant Enterobactericeae (CRE). CRE are bacteria that live harmlessly in the intestines of some people. However, when CRE moves outside of your gut, it can cause infections in your bloodstream, lungs, and urinary tract.
Unfortunately, CRE, a so-called “superbug,” is now resistant to virtually all antibiotics. As a result, up to half of infected patients die. CRE is particularly dangerous for people in hospitals and nursing homes who have weakened immune systems and use devices like ventilators or urinary catheters.
In their model, the researchers used data from long-term acute care hospitals in Chicago as baseline input for computerized scenarios. The first of the two new hypothetical drugs treated CRE bloodstream infections (BSI). The second was used to decolonize the bacteria in patients who were identified as CRE carriers but who didn’t have any symptoms.
Over the course of 30 different scenarios, the researchers varied the conditions, including the antibiotic used (either BSI treatment or decolonization), hospital occupancy rates, proportion of patients who carried CRE or had BSI infections, and the potential CRE transmission rates between individuals. As a control, they also simulated situations where no new antibiotic was used.
Overall, the decolonizing drug prevented more BSIs than the treatment drug and appeared to prevent up to twice as many deaths. Based on their assumptions, the researchers concluded that, in some situations, decolonization was also less expensive, costing about $4,000 per patient versus the nearly $55,000 needed to treat BSI.
“The current option for a person who is infected with CRE is to put them in isolation and try to prevent them from spreading it,” says Damon Toth, PhD, lead author of the study and an assistant professor of epidemiology at U of U Health. “That’s an imperfect solution. Instead, if a decolonization drug was available that could prevent individuals who are infected but not yet showing symptoms from transmitting it to others, that would be more ideal.”
The researchers acknowledge that some of their assumptions may not be accurate and could have affected the results. They also note that their results may not extrapolate to settings other than long-term acute care hospitals where patients are extremely ill and vulnerable to infection.
“Our results highlight the importance of taking into account the positive and potentially large spillover effects onto other individuals of infectious disease prevention efforts,” Nelson says. “Our hope is that these findings could lead to new policies to lower barriers for approval for these interventions and clinicians would be more likely to use them with their patients.”