Voices of U of U Health
Breakthrough Technology for Medical Students

Ultrasound technology has been part of clinical care for more than half a century. For most women today, it's hard to imagine going through a pregnancy without seeing the black-and-white images of a developing fetus, generated by the reflection of ultrasound waves. However, until recently, ultrasound machines were large and quite expensive, limiting their use throughout medicine.
Not anymore. Not at University of Utah Health.
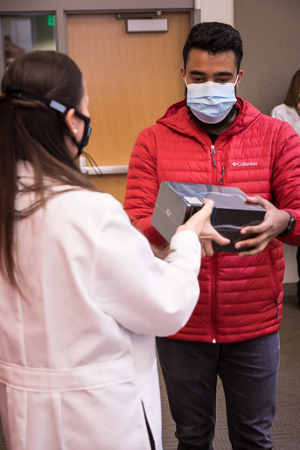
Here at the Spencer Fox Eccles School of Medicine (SOM), a batch of 500 handheld, point-of-care ultrasound devices (POCUS) were delivered in early November. They’re already in use, dispersed to students in every class. Every medical student now has one to scan patients, learn about anatomy and physiology, and view pathology in real time as they learn about it. In a short period of time—less than two months—students have enthusiastically let us know how well the probes help them in training and care for patients. These handheld devices have been described as a genuine breakthrough for facilitating medical diagnosis and therapy.
Now Standard Equipment
The devices consist of a small probe that transmits ultrasound images to a smartphone or tablet. The probes are close to the size of a cell phone or TV remote, making them highly portable. Students can take them anywhere. They can keep them in their bag so that, while learning, the device can be pulled out when they're trying to understand a concept and actually see that concept happening in real time in their own body. When they want to examine the pathology in a patient, they can just pull out their probe and put it on the patient. They can get ultrasound images right at the bedside without transporting the patient elsewhere for an ultrasound examination. This is a game changer for our students and for educating future physicians.
Answers at Bedside
Point of care ultrasound (POCUS) is performed right at the patient’s bedside. It can be performed with larger but moveable machines or with pocket-sized devices. The pocket-sized devices offer easier access, allowing physicians to scan patients and answer focused questions immediately as they arise. This allows routine screening for aortic aneurysms, dating the gestational age of a fetus, or looking for gallstones to be done conveniently in the clinic. The ability to answer specific questions quickly at the bedside saves time and health care costs, making it an attractive approach to patient care. For critically ill patients, POCUS allows physicians to answer questions that guide lifesaving treatment plans in patients who are too unstable to be moved for other imaging tests. These are further reasons why we have put a probe in our students’ hands and support them learning this skill early on.
For patients, these new portable devices bring a lot of screening and diagnostic capabilities right to their local clinic, wherever it is. Utah is a large state with low population density in most counties. Often, patients there must take time off of work to travel if they’ve been referred for imaging testing, which may not be available locally. To answer a simple clinical question, a low cost, ultra-portable handheld ultrasound device can answer that question immediately without requiring time off from work or long travel times. This is a huge win for patients in rural areas and yet another reason we are training the future physicians of this state to perform this valuable skill.
Training and Education
As for training physicians and students, the handheld ultrasound probes are very intuitive to use. The skill of knowing how and when to use POCUS is another skill altogether. This is why our medical students spend years developing this skill in a four-year integrated ultrasound curriculum. Each year, students build new layers of ultrasound skills to match their level of training and support learning other skills essential to being a good physician. Our goal is that our School of Medicine graduates physicians with a reputation for being skilled and comfortable with point-of-care ultrasound, which has the potential to improve health outcomes, especially in areas where access to ultrasound examination was previously out of reach.
Putting ultrasound probes in the hands of all students at Spencer Fox Eccles School of Medicine demonstrates the kind of cutting-edge innovation we are known for. These handheld devices are not common in U.S. medical schools. Ours is one of a very small handful of medical schools in the U.S. in which every student has their own ultrasound probe and a fully integrated four-year ultrasound curriculum. The devices mean better training for our medical students and better patient care for the people of Utah.
This project is supported by the Health Resources and Services Administration of the U.S. Department of Health and Human Services as part of an award totaling $13.4 million with 10 percent financed with non-governmental sources.