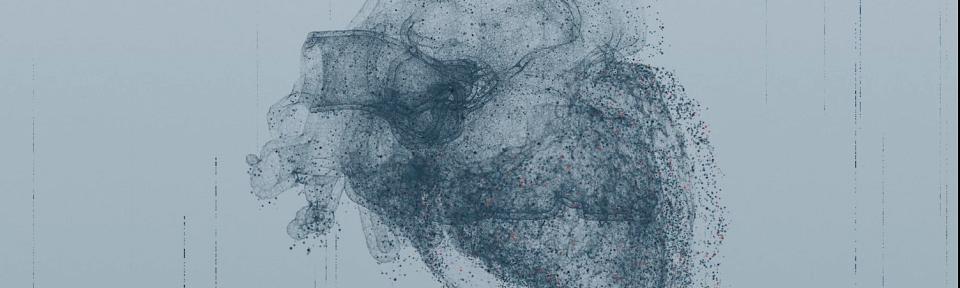
Can We Heal a Failing Heart?
Heart failure is a growing issue in the United States. About 6.2 million Americans now live with chronic heart failure, with 500,000 new cases per year and nearly 380,000 deaths attributed to the disease per year. Despite the increase in prevalence, there are few treatments specifically targeting the disease.
“I have to confess that, as a card-carrying cardiologist, current therapy is in the stone ages relative to medical therapy for many other diseases in cardiology and beyond,” admitted Robin Shaw, MD, PhD, director of the Nora Eccles Harrison Cardiovascular Research and Training Institute (CVRTI) at University of Utah Health.
Doctors often prescribe heart failure patients drugs such as beta-blockers, angiotensin converting enzyme inhibitors, and aldosterone inhibitors. But these medicines were developed for other conditions, such as high blood pressure, and not specifically for heart failure.
“What we don’t do a good job of is addressing the heart itself,” said Shaw. “How can we make this heart muscle better?”
"Current therapy is in the stone ages relative to medical therapy for many other diseases."
Shaw has spent his career finding ways to reverse these troubling trends. His research focuses primarily on complex proteins called cardiac ion channels. These proteins are responsible for propagating the electrical signals that make the heart contract, and changes to their function or distribution across the heart’s surface can contribute to heart failure. Shaw’s lab studies how cardiac ion channels are formed and how they are targeted to specific subdomains of cardiac cell membrane in both healthy and failing heart muscle. This “cell to bedside” approach is designed to develop novel diagnostics and therapeutics for failing hearts.
He is one of the many scientists at U of U Health’s CVRTI dedicated to answering vital questions about how to heal a failing heart. With a staff of nearly 100 researchers spread among 14 laboratories, the CVRTI is the largest free-standing collection of cardiac muscle biology, metabolism, and electrophysiology researchers in the country.
Among the institute’s recent discoveries spearheaded by Shaw is that heart failure progression is associated with decreased levels of a protein called cardiac BIN1, or cBIN1. Shaw’s studies have also revealed the role that cBIN1 plays in individual heart cells. The protein forms little baskets, or “microdomains,” that collect and organize the important proteins that make a heart contract and relax.
He is one of the many scientists at U of U Health’s CVRTI dedicated to answering vital questions about how to heal a failing heart. With a staff of nearly 100 researchers spread among 14 laboratories, the CVRTI is the largest free-standing collection of cardiac muscle biology, metabolism, and electrophysiology researchers in the country.

Among the institute’s recent discoveries spearheaded by Shaw is that heart failure progression is associated with decreased levels of a protein called cardiac BIN1, or cBIN1. Shaw’s studies have also revealed the role that cBIN1 plays in individual heart cells. The protein forms little baskets, or “microdomains,” that collect and organize the important proteins that make a heart contract and relax.
In preclinical studies, Shaw and his colleagues have been attempting to restore levels of cBIN1 via gene therapy. Results show that upon directly injecting the protein into the hearts of mice, heart failure can be reversed, and mortality reduced.
Shaw and his team hope to launch clinical studies in humans in the next three to five years.
“We’re very excited,” Shaw said. “This would really represent a first in class therapy for heart muscle, which is of enormous importance to all of us.”
-written by Chris Palmer
Learn more about Shaw’s research and CVRTI.
The video was filmed at an event held for U of U Health Partners. The event and video were produced by Ben Tomlin.