

Author: Julie Kiefer
Discoveries from the laboratory of Stefan Pulst, Dr Med, on a rare disease, ataxia, has led to a potential treatment for another devastating neurological condition, ALS. Photo credit: Charlie Ehlert.
More than 25 years in the making, scientific discoveries made by Stefan Pulst, MD, Dr Med, and his research team have reached the milestone of entering human clinical trials with a unique treatment for amyotrophic lateral syndrome (ALS). The experimental drug is one of a new class of next-generation therapies that address the root cause of the disease—the genetic code—and show promise in alleviating previously untreatable conditions.
It’s an encouraging step forward for ALS, or Lou Gehrig’s disease, a rapid and progressive loss of function of cells in the nervous system. Today, patients have an average life expectancy of just two to five years after diagnosis, and no medications can slow or stop the disease.
“This is a sea-change,” Pulst says. “It is the first compound of its kind for all types of ALS, genetic and sporadic. We hope that in 10 years we’ll be talking about this like we do targeted therapies for cancer today.”
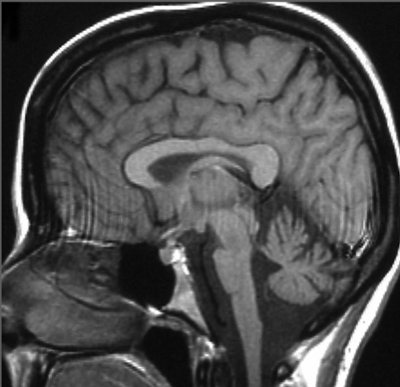
In the 1990s, Pulst couldn’t have known that meeting a family with a different nervous system disorder—ataxia—would set forth a path to the novel trial therapeutic for ALS. Upon learning about the family from a medical colleague, Pulst flew across the country from Cedars-Sinai Medical Center in Los Angeles, where he was chair of neurology, to upstate New York to examine family members and gather samples for analysis. The encounter launched a five-year-long investigation culminating in discovery of changes in a gene, ataxin-2, that caused their “family curse,” now called Spinocerebellar Ataxia type 2. The same genetic condition was also found in unrelated families around the world.
A decade later, Pulst moved to U of U Health as chair for the Department of Neurology, where he pursued research to gain an in-depth understanding of what goes wrong in the body during the course of disease. With his close collaborator Daniel Scoles, PhD, associate professor of neurology, he developed mice with an ataxia-like condition, providing a means for discovering genes and biochemical pathways that become perturbed over time. The disease model also served a second critical role: Because it expressed the mutant human ataxin-2 gene, it became a tool for testing gene-targeted therapeutics.
This is a sea-change... We hope that in 10 years we’ll be talking about this like we do targeted therapies for cancer today.
Stefan Pulst, Dr Med
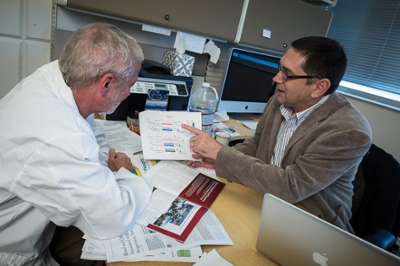
Pulst and Scoles collaborated with Ionis Pharmaceuticals to pursue a novel treatment approach that began to show promise for other neurodegenerative conditions. They demonstrated that a type of drug, known as antisense, reduced expression of the ataxin-2 gene and slowed progression of the animals’ ataxia-like condition. Mice performed better in balance and coordination tests and showed signs of recovery at the cellular level. The antisense drug is a chemically synthesized, DNA-like molecule that targets ataxin-2 mRNA, resulting in its destruction.
In a surprise finding, a second study showed that a similar antisense drug against ataxin-2 also improved the health of mice with an ALS-like condition. In this case, the effect was indirect, reducing toxic clumping of another protein known to be involved in causing ALS. The treatment dramatically extended the lives of the ALS mice.

“This was a proof-of-concept that these compounds could become the basis for new therapies for neurodegenerative diseases, which so far have been largely impenetrable,” Pulst explains.
With support from the National Institutes of Health, Pulst, Scoles, and Ionis Pharmaceuticals further refined the treatment, finding an antisense drug that performed well in animal studies with unparalleled safety and effectiveness. Based on these results, the U.S. FDA gave clearance for human trials. Phase 1 clinical safety trials of the drug, called BIIB105, are sponsored by Biogen and begin enrolling patients on September 2.
“One of my professors told me it is rare for someone to make a meaningful difference in science,” Scoles says. “But we never stopped trying. Hopefully this drug makes a significant difference.”
Photo credits (except MRI image): Charlie Ehlert.