
Making Sense of the Numbers Game
Author: Kamryn Broschinsky
Using Twitter, researchers learn how patients take diabetes care into their own hands.
"We are not waiting.” This simple phrase holds a lot of weight. Historically uttered in countless contexts, it was used at a 2013 diabetes “hacker” convention as a rallying cry and reminder to the diabetes community that they are in control of their own health. The act of turning the phrase into a Twitter hashtag gave the new movement the momentum it needed. An international community of patients, caregivers, friends, and family members congregated around one simple desire: to improve the quality of life for people living with type 1 diabetes by using open artificial pancreas technology.
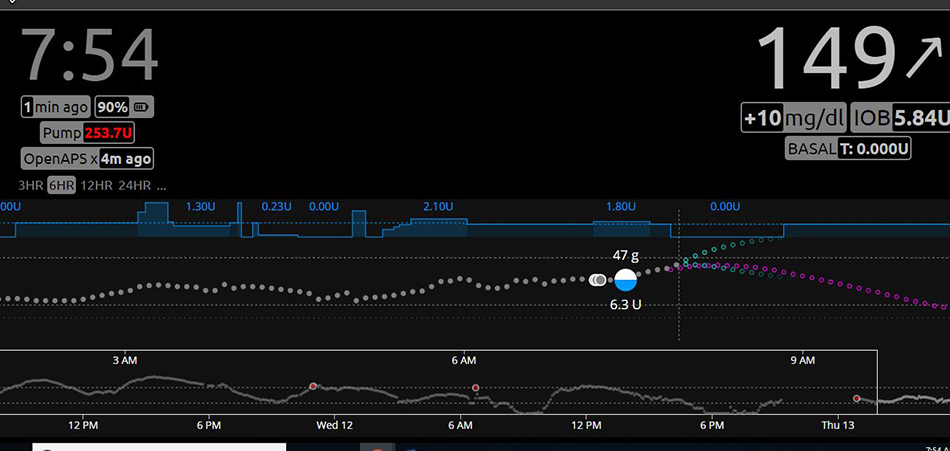
Open artificial pancreas (OpenAPS) technology consists of a hacked insulin pump, continuous glucose monitor (CGM), and a microcomputer combination that work together to minimize the dangerous blood glucose variability caused by the condition. Unlike the Food and Drug Administration (FDA)-approved artificial pancreas system that is now on the market for upwards of $5,000, the cost of the patient-hacked OpenAPS system is only in the hundreds of dollars, but is neither FDA regulated nor approved.
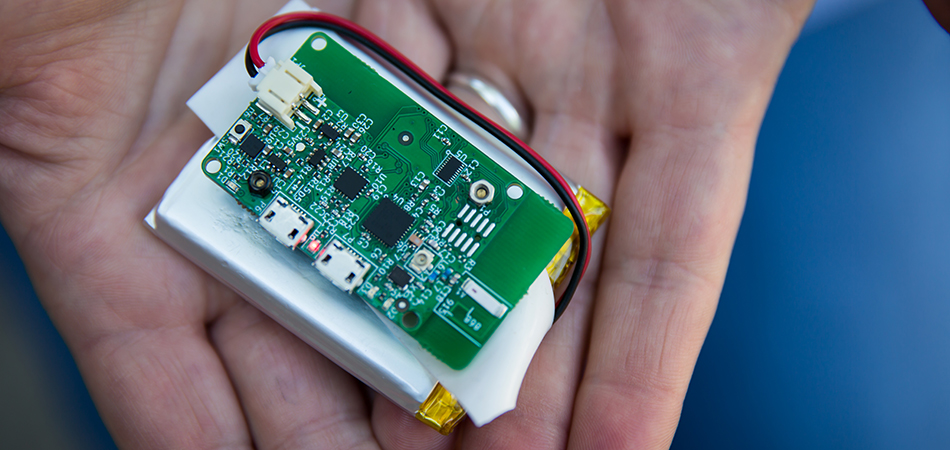
Medical devices are usually designed in a way that prevents users from modifying them. But what may be a minor inconvenience for some people may be a life-threatening design flaw to others. For a father who needs to remotely monitor his four-year-old’s blood sugar levels, or for a woman who sleeps through low-sugar alerts, figuring out how to modify their medical devices was worth the risk. Thus, the OpenAPS movement was born.
"The ultimate patient-centered care is through these citizen scientists because they’re creating what they need," said Michelle Litchman.

Michelle Litchman, a researcher and nurse practitioner with University of Utah Health, prefers the word maverick when describing the hackers of the grassroots movement.
“The ultimate patient-centered care is through these citizen scientists because they’re creating what they need,” Litchman said. “Not every patient is exactly like one other patient; I think it is really powerful that we’re identifying what patients really find valuable.”
Litchman — whose current research revolves around the intersection of diabetes health, community and technology — wanted to take a closer look at how people use social connections to support their diabetes management. She analyzed thousands of tweets with the #OpenAPS and related hashtags, that had been posted by patients and users, caregivers and care partners to determine how they are compensating for a health system that has failed them.
Diabetes devices, needles, pens, pumps, are hardly built in a one-size-fits all fashion, but Litchman’s research on Twitter provided an echo chamber to hear how Open APS — a more adaptable alternative — is making waves.
A CALCULATED RISK
Mikel Curry was diagnosed with type 1 diabetes when she was three years old, she has never known a life free of the disease. In the early days after her diagnosis, there was no fancy technology and Mikel had to rely on a urine sugar testing kit; now at age 43 she is a living timeline of the rapidly evolving landscape of diabetes management.
Controlling the disease is like walking on a tightrope, explained Mikel. Taking too much insulin can cause a severe drop in blood sugar (hypoglycemia) which can lead to seizures, a diabetic coma, and even death. Too little insulin can trigger a life-threatening condition known as diabetic ketoacidosis, in which the blood becomes dangerously acidic. Despite significant progress over the years, today’s means for maintaining the balancing act are still not good enough, she said.
"Controlling the disease is like walking on a tightrope," said Mikel Curry. "Trusting a machine was a leap of faith."
Initially, Mikel was hesitant about joining the OpenAPS movement, but her husband Jason helped convince her of the value. And once she did, it changed her life.
“My initial drawback was there’s no way I can do this, I’m not a biohacker, I’m not a programmer or a bioengineer,” Mikel said. Placing her life in the hands of a system that takes over most decision-making aspects of her health was no easy task, from either a skill or confidence perspective. “Trusting a machine was a leap of faith,” she said.

The results of Litchman’s study echoed Mikel’s sentiment, initial hesitation was not uncommon.
“There is a fear of not being able to set up the technology correctly, because you don’t have a certified diabetes educator who can walk you through all the ins and outs of setting up like you would for an insulin pump or maybe a continuous glucose monitor,” she said.
With no background in biomedical engineering and yet trying to write programming code Mikel’s health and well-being would depend on, she was understandably overwhelmed. But she had the support and encouragement necessary to take the leap.
In a world of artificial hearts and lab-grown livers, writing code for your own medical device isn’t all that strange. Diabetes is a numbers game. Blood glucose, blood pressure, cholesterol levels and finances all play crucial roles in managing diabetes, and computers are good with numbers. Instead of Mikel having to making hundreds of decisions a day about her health, every minute the machine would make one for her.
IT TAKES A VILLAGE
The prevalence of peer support — a pillar of the OpenAPS movement — is a common theme among users. Litchman is struck by the supportive nature of the movement, and considers the community as one of the most compelling aspects of the technology.
Social media has evolved into a powerful means of creating diverse, global partnerships. An online presence can provide support groups to people who previously had no access to one, and who desperately needed it. Twitter was Litchman’s platform of choice as it offered her real-world surveillance of this peer health exchange.
While most existing research around OpenAPS focuses on the compositional aspects, such as technical development and implementation, Litchman’s project uniquely focuses on the online peer health aspect. She analyzes how the technology is received by community, the impact, interactions, and outcomes.
Litchman’s study reflected a significant trend within the movement. The marketplace of ideas helped to make up for the lack of formal instructions or training for Open APS. Users must rely solely on the collective intelligence of the community. But even the lack of “formal instructions” may offer a collaborative advantage by bringing different tips, tricks and perspectives into one melting pot.
“There’s definitely a community support group and we all want to share… we know how much time it takes to keep yourself in good control, and we all want to lessen that burden,” Mikel said. “Everybody who is using it wants to help someone else.”
Twitter was the perfect playing field as it also offered Litchman real-world surveillance and candid insights about the benefits and consequences.
At the minimum, knowing how patients are making up for deficits in their care gives Litchman and other health care providers an honest glimpse of their world. Knowing the lengths patients go to could ultimately prod the health care system into find ways to meet their needs.
“Citizen scientists from all over the world have come together to share solutions about a problem they’re facing with regards to diabetes management,” Litchman said. “And they’ve created these solutions that can then be tailored for different individuals, technologies, needs and desires.”
For people living with a disease that demands their constant attention, efficiency is everything. This applies to not only members of the diabetes community, but for anyone living with a chronic condition that requires ongoing medical attention. One day there may be new technologies that open doors previously closed to people living with diabetes. But for now, OpenAPS, patient-driven care, confidence and community have a permanent home together.
Banner image of Mikel Curry. Credit: Charlie Ehlert