

Under Pressure: Researchers Search for New Glaucoma Treatments
A team of scientists at University of Utah Health work to develop glaucoma therapies that treat pressure in the front of the eye and prevent damage in the back of the eye.
Author: Stacy Kish

Barbara Van Asdlan has led an adventurous life. Using quick, active hand gestures, she explains her history as a nurse at Landstuhl Regional Medical Center, Germany. Her time in Europe sparked her love of travel and learning about new cultures and communities. Today in her mid-70s, Barbara has not slowed down, but a diagnosis of glaucoma did give her pause.
“When I was told I had glaucoma, it was shocking and devastating,” Barbara said. “I knew if I didn’t get it treated I was going to go blind. Nothing could be as bad as being blind.”
A Slow Descent into Blindness
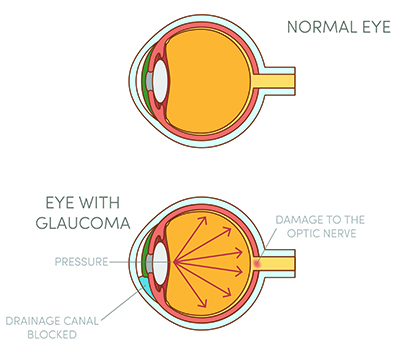
Glaucoma is an insidious disease that develops slowly over time with few early warning symptoms. Previous research has linked the disease to abnormal internal eye pressure.
As the pressure builds, cells within the retina, the thin slip of tissue that lines the back of the eye, begin to die. The retina is critical for vision. It intercepts and transfers light into electrical signals that the brain interprets as visual images. The retina is a tapestry of different cells, including retinal ganglion cells, responsible for sending projections to the brain. When the retinal ganglion cells die, they are lost forever, leading to progressive and irreversible vision loss.
Barbara did not sit quietly after her diagnosis. She took matters into those active hands to ensure her love of travel would not be robbed from her life. At this time, glaucoma treatments are limited to eye drops, laser surgery, and conventional surgery. While these options prevent additional vision loss, they do not restore or improve vision.
Barbara tried different eyedrop treatments, with mixed results. But for her, the out-of-pocket expense of the medications was the biggest hurdle to overcome.
“My Medicare didn’t cover enough of the cost,” she said. “When you are elderly that is when you need the care the most.”
She took a step that most people would choose to avoid. Barbara opted for surgery that could reduce or eliminate the need for the expensive medications.
A friend recommended that Barbara see Craig Chaya, MD, at the John A. Moran Eye Center. Dr. Chaya recommended she try surgery using a XEN® gel stent, a tiny tube the size of an eye lash. Once inserted, the stent offers a safe and effective way to lower eye pressure.
“Dr. Chaya listened to my concerns,” Barbara said. She appreciated the time he took to explain her options and put her mind at ease. “During my surgery, he described everything that was happening as it happened.”
Barbara’s surgery has proven to be a success, but researchers at University of Utah Health continue to look for more effective treatments that could reduce the need for patients, like Barbara, to seek surgery.
In Search of the Molecular Bridge
David Krizaj, PhD, professor of Ophthalmology and the John Frederick Carter Endowed Professor of Ophthalmology at U of U Health, and his team are particularly interested in the millions of retinal ganglion cells woven into the tissue along the back of the eye.
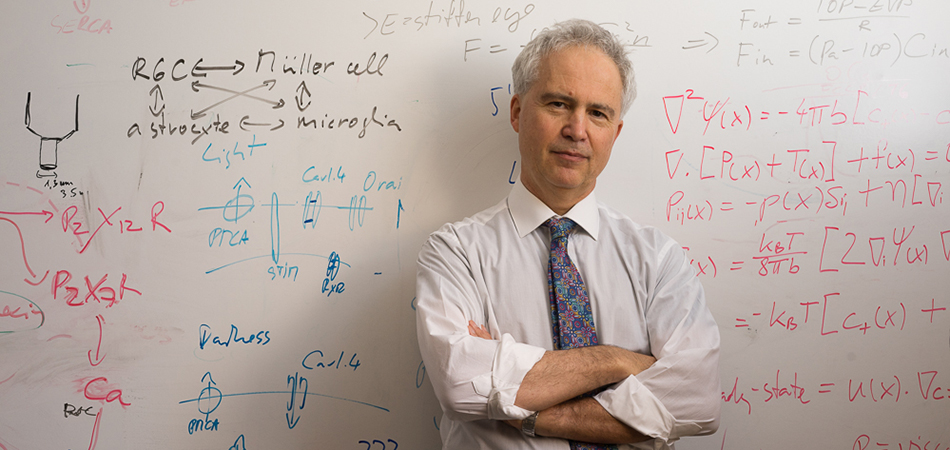
“These nerve cells function as projectors that interpret specific features of our visual environment and communicate to the brain,” said Krizaj.
But exactly how pressure affects these nerve cells remains a mystery. Krizaj focused on the environment in which the cells live for clues.
“I think of each cell as an organism that wants to participate and understand what is going on in the world around it,” he said. His group is focused on finding how cells obtain information, like pressure, about the surrounding environment.
Krizaj and his team began to sift through the eye’s cellular mechanisms to identify the molecular bridge that allow multiple cells to coordinate and collaborate as they respond to pressure. With this information, he hopes to develop strategies that will both lower eye pressure and protect pressure-sensitive ganglion cells from injury.
Ocular Pressure Cuff Yields Clues
In his studies, Krizaj turned to mechanobiology, an emerging field of science at the interface of biology and engineering that explores how physical forces affect cells and contribute to the development of disease.
Using high-speed pressure clamps, his team applied precise and defined pressure pulses to individual retinal ganglion cells. With this explicit stimulation, they were able to determine the threshold pressure for individual cells.
Lurking within the retinal ganglion cells, Krizaj found a pressure-sensitive molecule that is not found in other neuron cells in the eye. This particular molecule is also found in inflammatory cells that accelerate neuron degeneration.
“We could see that retinal ganglion cells are incredibly sensitive to mechanical forces, like pressure,” he said.
Krizaj and his team were excited to discover that this same ion channel that confers pressure sensitivity to ganglion cells also appears to regulate pressure itself. In a healthy eye, this ion channel is kept in check with another protective molecular mechanism. In the absence of this check, the activated channel begins to cascade out of control, ultimately leading to pressure elevation and ganglion cell death.
“We are currently developing a novel glaucoma drug that could both lower the pressure in the eye and suppress the sensitivity of cells affected by pressure,” Krizaj said.
Krizaj is hopeful that this approach could help patients, like Barbara with open-angle glaucoma, the most common form of the disease that affects primarily older adults. If successful, it might also help patients who experience other blinding diseases, like diabetic retinopathy and macular edema, which are associated with excessive swelling.
New Therapies on the Horizon
Krizaj understands the importance of transferring his research from the lab bench to the bedside and is working with the Center for Technology and Venture Commercialization at University of Utah to help advance the development of this therapy.
“This research is the holy grail of glaucoma,” said Leena Bhoite, PhD, technology manager at TVC. “We are here to provide our researchers, like Dr. Krizaj, with all aspects of innovation management that they need.”
With TVC serving as a business catalyst in the regional ecosystem, Krizaj and the University of Utah have licensed the technology to Aspectu Therapeutics to help guide these compounds to Phase-1 clinical trials, which are anticipated in the next few years.

Barbara is all in favor of the research being conducted at U of U Health. “If we didn’t have research where would we be?” she asked. “We would be back in the dark ages.”
Following her surgery, Barbara still needs her glasses, but she has no problem getting around town. Today, she has her eyes set on new, exotic locations to explore.
“I still want to take a trip on the Trans-Siberian Railway or even the Orient Express,” she said.
This project received preliminary funding from the University of Utah Center for Clinical and Translational Science, the U of U Health Neuroscience Initiative, and a USTAR Technology Acceleration grant, as well as the Willard L. Eccles Foundation and the National Institutes of Health and the Glaucoma Research Foundation.