
Scientists at University of Utah Health have developed a test that can quickly identify populations that had been recently infected with cholera. The new test can be easily deployed in the field as a first step in deciding on the most effective way to curb the spread of disease.
Cholera is a debilitating diarrheal disease that remains a major public health concern, especially when sanitation is disrupted and access to clean water limited in war zones and disaster areas. Transmitted by food or water contaminated by Vibrio cholerae, the disease can kill within hours without treatment. While a vaccine is available, the World Health Organization estimates that cholera continues to affect as many as 4 million people every year, resulting in 143,000 deaths worldwide.
“For a place like Haiti or Yemen where so many people are at risk of getting cholera, it may be impossible to focus resources, like the cholera vaccine, on everyone,” said Daniel Leung, MD, MSc, an assistant professor in the Division of Infectious Diseases at University of Utah Health.
Public health officials survey a region to identify vulnerable pockets of the population, but current surveillance methods still rely on reports of abrupt bouts of watery diarrhea confirmed by infrequent laboratory results. Blood contains the information that scientists need to identify the presence and extent of cholera in a region, but the logistics behind drawing, storing, and transporting tubes of blood in harsh conditions proves challenging.
“When you arrive at an ongoing epidemic, you need to have a way to quickly measure a certain level of antibody in the blood,” said Leung. “If cholera already passed through the population, they are protected, but vulnerable residents need to be vaccinated immediately.”
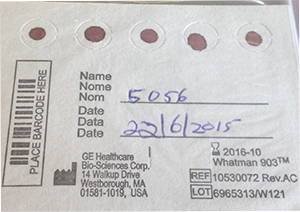
Leung and colleagues at U of U Health developed a field-friendly surveillance method that only requires filter paper and a lancet. With a prick of the finger, a few drops of blood are collected and dried on the filter paper. Using standard laboratory procedures, the dried blood spots are subjected to a simple assay, as well as conventional spectrophotometric methods to identify cholera-specific antibodies.

The team validated this technique using samples collected at a displaced persons camp in South Sudan. Blood draws and blood spots were collected from participants before and several weeks after receiving the cholera vaccine. Patients that receive the vaccine will have a higher level of cholera antibodies in their blood, similar to surviving a bout of the disease.
The dried blood spots were stored in field conditions in Africa for months before being shipped under ambient temperatures to the U of U Health laboratory for analysis. Despite the rugged conditions surrounding collection, the samples retained functional antibodies to identify cholera successfully.
Looking for bug in the stool or collecting tubes of blood is not easy in these difficult settings where cholera thrives,” said Leung. “This simple field test is one component of a tool kit that we are developing for field cholera epidemiology.
Leung collaborated with Medecins Sans Frontieres (Doctors without Borders), the South Sudan Ministry of Health, and World Health Organization officials to gather samples in South Sudan, some of whom are already considering use of this field test to help triage interventions to prevent the spread of disease.
This work was supported by The National Institute of Health, The Bill and Melinda Gates Foundation, the Intramural Research Program of the National Institutes of Health, and Margaret A. Cargill Foundation grants to WHO.