
Author: Michael Mozdy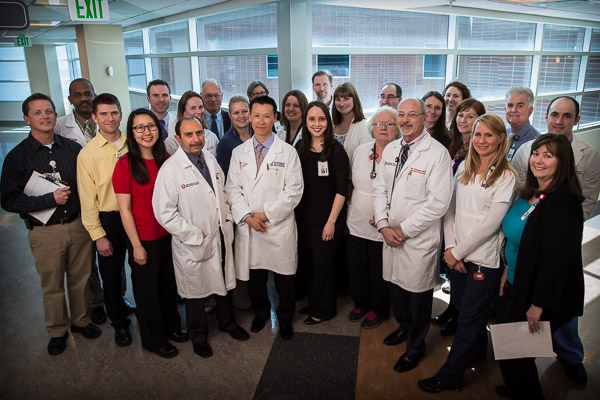
Editor's Note: on Tuesday, May 20 the transplant team at University of Utah Health "live Tweeted" two successful kidney tranplant surgeries as part of an ongoing effort to raise awareness about the importance of organ and tissue donation. The story below, taken from the University's employee intranet, details the University's Transplant Value Initiative.
At the end of March, University of Utah Health tried something new with a kidney transplant patient: after the transplant surgery, the patient bypassed the Intermediate Care Unit (IMCU) and went directly to a general nursing recovery unit (the SSTU). To those unfamiliar with the intricacies of transplant, this might not seem like news; but once you understand the complexities of transplant, this is a significant shift in the way we're handling patients.
Many people think of transplantation as if our bodies were cars and we just need to replace a single part, say the catalytic converter. Of course, we're much more complex than machines, and that organ in need of transplant can impact all of the other systems in the body. Conversely, other health issues can impact how successful transplanting that one organ might be. If a person is obese, or has a history of smoking, for instance, the care team needs to pay close attention to heart and lung issues before and after transplant.
The list of things that could potentially go wrong is daunting, to say the least. This is why most transplant programs send patients to an ICU directly after surgery to provide a high level of watchfulness and care.
Success Starts Before Patients Even Get Here
Because we're attuned to all of the potential issues with transplantation, the University of Utah Transplant Center gives patients the royal treatment from the very beginning. Patients are assigned a "care concierge" who is a highly trained transplant nurse. This guide stays in close contact with patients' referring providers to complete a comprehensive pre-transplant checklist. All of the tests are ordered and the specialists are lined up to meet with patients when they step through the door for the two-day process of preparing for a transplant.
"We are fortunate to have not just a multifaceted core transplant group," says Robin Kim, MD, Director of the Transplant Center, "but also a multidisciplinary 'second layer' of providers who make sure that we pay attention to everything we need to." This second layer of the care team consists of cardiologists, interventional radiologists, hepatologists, oncologists, pulmonologists, and more.
Just as important as this cross-trained multidisciplinary team working with patients before and during the transplant is the cross-training of nursing teams caring for them during their recovery. The IMCU, SICU, and SSTU all work seamlessly to move patients to the units where they will receive the appropriate level of care. "It's a very fluid process," says Kim, and the close relationship between the nurses on these units has enabled this new process of moving patients directly to the SSTU.
Nursing staff and leadership in the SSTU have developed such a level of care, knowledge, and specialization for transplant patients that they are able to receive these patients after surgery and provide the level of care they require. Colline Prasad is the nurse manager on the SSTU, and has worked hard to develop not just the skills of her nursing staff, but also a great relationship with the Transplant team. "The kidney, pancreas, and liver teams are just fantastic--we have a great relationship with the doctors. They have a lot of faith and trust in us to care safely for their patients, and it's so nice to have them be engaged nursing advocates."
"The reason we want to avoid the ICU is twofold," notes Kim. "First, there are significant costs to the patient and to our system when we use an ICU, and second, it frees up the ICU to handle the sickest patients who need that level of care." Kim and the transplant team hope that this new process will be able to be used for most kidney transplant patients. This is their way of engaging with process improvement methodology to increase value in our system: costs are lowered while quality remains high.
Of course, a good value-driven care project analyzes the entire process to ensure that all of the supporting steps will make a process change successful. The Transplant team has made sure that their daily processes support this change in where patients wake up after surgery. "Everyone is aligned with providing the right level of care," says Kim. The Transplant physicians have daily conversations with the directors and attending physicians on the IMCU, SICU, and SSTU. What's more, every day at 2 p.m. a multidisciplinary team rounds with the nurses on each unit, bringing together physicians, pharmacists, coordinators, dieticians, nurses, and more.
This care team is focused on just one thing: "Everyone involved has been making great joint decisions based completely on what's the best thing for our transplant patients," says Kim proudly.
And this is just one of three recent value initiatives that the Transplant Center has done in the past year.
The Shorter the Stay, the Higher the Value
A second project is the Transplant Center's length-of-stay (LOS) initiative. It's no secret that patients would prefer to spend less time in the hospital rather than more time. It also turns out that the risk of getting a hospital-acquired infection goes down, as does the cost to the patient and the system. The Transplant team identified a number of steps to help patients get out of the hospital sooner: allowing them to progress to a new diet sooner, encouraging them to start walking sooner, educating them sooner on their complex immunosuppression regimen, removing catheters and lines earlier, and creating a seamless scenario where their outpatient care is scheduled and easily understood.
Another notable change the team needed to make was to prepare patients mentally. "We expect you to do well enough to leave on day three or four," says Kim, "it's all about expectations."
This UHPP-funded initiative saved roughly $500,000 over the course of a year and kept the quality of care very high.
Smart Use of Meds
A third value initiative exemplifies what is different about working at an academic medical center like the University of Utah, where research plays an important role in being on the cutting edge of care delivery. The Transplant team embarked on a one-year study to see if an alternate immunosuppression medicine would be just as effective as the traditional, more expensive medicine in patients. They found that that it was not only just as effective, but perhaps even more effective than the more expensive medicine. This project also projects to save about $500,000 per year, meaning it's cost effective while creating a better outcome for our patients.
Team Transplant
Dr. Kim is quick to pass credit to the whole care team. "None of this could have been done without the nursing leadership, our coordinators, our pharmacists, hepatologists, nephrologists, and surgeons," he says. Everyone is valued for the ideas they can bring to the table, both in day-to-day care and in long-term value projects. The Transplant team is setting the bar for defining how true collaboration among varied professions can result in better care for patients and better value for our system.