Author: Stephen Dark
When Jorgen Madsen came out to his family in late 2015, his father told the 23-year-old medical student a cautionary tale about the only gay man he knew. In the wake of his HIV diagnosis, his father's friend had been ostracized by the small, rural Utah town where Madsen had grown up. Only seven people went to his funeral.
"The story of my dad's friend made HIV very scary for me personally,” Madsen says. “The way that town reacted: people don’t talk about him; he’s one of those secrets. I didn’t want that to be me.”
Madsen approached gay life with trepidation. After learning about the dating app Grindr, he downloaded it, only to be traumatized by the dozen men immediately asking him for sex.
Madsen took the world of dating very slowly. His first kiss with a boyfriend at the end of their third date was an emotional revelation. “I’d never felt anything more pure, more honest,” he says. Shortly after that date, Madsen went to the hospital for treatment on an old bone break that had painfully flared up. This was the first time he identified himself as gay. “The experience was less than ideal,” he says.
Through the walls, he heard the nursing student who had taken down his details tell the doctor, “I’m afraid he’s at high risk, being homosexual.”
Medical staff grilled the terrified student about his sexual activity, even though it only amounted to a lip-locking farewell at the front door. “They didn’t believe me,” he says. “They still screened me for everything. I felt so vulnerable.”
An attending opened the door and shouted, “We need an HIV test in here.” Madsen sank further down into his chair.
They told him he should start taking PrEP, which stands for Pre-Exposure Prophylaxis. Essentially a one-pill-a-day intervention, it has proven up to 95 percent effective against HIV infection. A Lancet study on “rapid, targeted, high-coverage roll-out” of PrEP in New South Wales published in fall 2018 made international headlines, revealing that PrEP usage led to “a rapid decline in HIV diagnoses.”
When Madsen asked why the staff thought he should go on PrEP, they replied, “Well, you engage in risky behavior.”
It was just a kiss, he thought.
While highly effective in combatting HIV, PrEP is also very expensive. Madsen would have to pay $1,500 a month, half of which his insurance would then reimburse. As much as he wanted to take PrEP, he couldn’t afford it. “I felt like a hypocrite being a medical student and not doing everything I could to be safe,” he says.
Afterwards, he sat in his car in the hospital parking lot, humiliation washing over him. As he stared numbly out of the window, he cried.
Over the next two years, Madsen got a crash course in the paucity of LGBTQ health resources in Utah. He joined forces with two doctors at University of Utah Health, Susan Keeshin, MD and Adam Spivak, MD, along with a fellow medical student, Julie Weis, and the local nonprofit Utah AIDS Foundation, to improve health care for the LGBTQ community.
Their main efforts laid the groundwork for what at that time was only the second free PrEP clinic in the U.S. Madsen and his allies found that while it took a collective effort of passionate, activist-minded medical staff to stake out a new frontier in LGBTQ health culture, inside the clinic it came down to communication between providers and patients to realize their dreams of change.
Madsen and the rest of the clinic’s leadership had four goals for the HIV prevention clinic: to serve the LGBTQ community, to educate the community about safe sex, to build trust between patients and LGBTQ-allied and gay medical professionals, and to educate the medical community about LGBTQ health issues. Part of that last goal was learning how to take a patient’s sexual history in a non-judgmental manner. That involves recognizing the role humility plays in HIV care, Keeshin says, especially given the fact that patients are typically underserved. Doctors who work with them, “have to check race, sexuality, and privilege at the door,” she says, “whereas a lot of other specialties you don’t.”

Volunteer staff at the end of the PrEP Clinic's inaugural day. Credit: Jorgen Madsen
The clinic is a space where we can talk about the excitement of a date they had, or how the family is reacting to coming out.
In March 2018, the clinic began opening its doors every other Saturday morning from 9 a.m. to 1 p.m. Spivak and Madsen (the dreamers, the big-vision guys) and Keeshin and Weis (the practical engine of the clinic that keeps it motoring) volunteer their time, along with a rotating handful of medical students, several case managers, and a physician’s assistant.
In just six months, the skeletal crew squirreled away in the back of the Redwood Health Center on Salt Lake City’s west side has been all but overwhelmed by its own success. Ninety-eight percent of their patients are young gay men, and close to 40 percent identify as Latino, so the clinic has reached the most at-risk populations with little more than word of mouth.
This, however, is just the beginning. One Voice Recovery director Patrick Rezac told Keeshin he’s tried unsuccessfully to get the more than 1,000 patients at his needle exchange and addiction recovery program to go to the clinic. A mobile clinic, they agreed, might well cover that gap.
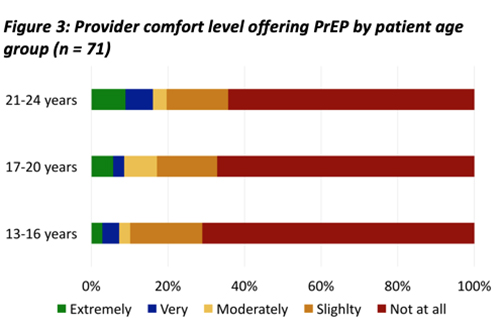
Provider comfort with youth access to PrEP. Source: Keeshin, 2016
The need for the PrEP clinic was apparent in a 2016 survey conducted by Monica Schwarz Josten, MD, and Keeshin. It showed, Keeshin says, that “primary care providers are very uncomfortable talking about sex,” and did not screen young patients for HIV infections. The majority of survey respondents took the view that their youthful patients weren’t sexually active. Yet results revealed that, in Utah in 2016, youth from ages 15 to 24 accounted for more than half of sexually transmitted infections and 21 percent of new HIV infections.
One reason doctors won’t prescribe PrEP, Madsen argues, is that they feel “morally opposed” to it. “They feel it increases promiscuity, increases risky behavior, and doesn’t protect against other STIs [sexually transmitted infections],” he says, “since patients taking PrEP are less likely to use condoms.” While some health officials who battle sexually transmitted infections [STIs] in the gay community link spiking STI rates to PrEP use, Madsen says such concerns are a fallacy. He points to studies showing that STI incidence decrease because patients, in order to keep receiving PrEP, have to get tested for HIV and STIs every three months.
From the beginning, Madsen and his cohorts were determined to make the clinic an oasis of tolerance and empathy. Along with PrEP and STI education, they provide peer counseling for patients struggling with stigma, isolation, and depression. “This is a population that’s already marginalized,” Madsen says. “The clinic is a space where we can talk about the excitement of a date they had, or how the family is reacting to coming out.”
The Utah Aids Foundation (UAF) has served as the clinic’s strongest ally, Madsen says, referring uninsured patients to them and helping to organize fundraising events. UAF HIV prevention coordinator Daryl Herrschaft credits Madsen’s persistence for providing UAF and the gay community access to decision-makers at University of Utah Health who were able to put this clinic into place. “Madsen was the driving force turning the clinic from a concept into a reality,” Herrschaft says.
Even when Madsen’s sitting still, his long legs scissor in one direction, then swing back; his energetic enthusiasm is contagious. “When you work with him, you feel compelled to try to follow through what he’s planning,” Herrschaft says.
That same zeal for PrEP access is apparent in the clinic’s other co-founders: Spivak advocates intensely for the underserved, while Keeshin’s steely focus helps to marshal the flow of the clinic’s patients. Part of the clinic’s culture is to be realistic about people’s sexual behavior. “People still do practice high-risk sexual behavior,” Spivak says. “That’s the nature of life. If someone wants to use PrEP instead of a condom, we can talk about that decision. We know PrEP works. That’s what I care about: preventing HIV.”

Julie Weis Credit: Jen Pilgreen
AN EMOTIONAL CONNECTION
In 2015, Julie Weis was living in Seattle, pursuing a Master’s in public health, when she learned that her dad had been diagnosed with brain cancer. Then 29 years old, she decided to return to Utah to care for her dying father and signed up for medical school at the U. In her first year, she met and befriended Madsen, who also identified as LGBTQ. (“It’s the least interesting thing about me,” she says with a laugh.)
When Madsen shared his frustrations about the lack of dedicated resources and treatment for LGBTQ members with Weis, he also talked about his idea for a free PrEP clinic. Weis was thrilled. While insurance coverage had improved, she believed more work was needed: “There’s a lot of people who are most at need of it who don’t have insurance at all,” she says.
In summer 2017, Madsen’s frustration with the lack of resources addressing LGBTQ health issues hit a boiling point. He emailed Spivak, who teaches a four-hour HIV class to medical students at the University of Utah, for help addressing “what barriers our community is facing with the LGBT community and medicine,” Madsen wrote, “and what we could do as students to be involved.” Spivak was excited by the idea, one that had gripped his imagination when it was first suggested to him by a former Utah Aids Foundation employee.
A Maryland native, the 43-year-old Spivak was painfully aware of the socioeconomic differences dictated by a change in zip code from the comfortable middle-class neighborhood where he grew up and Baltimore’s downtown, where he first worked as a doctor. “All of my patients were black, largely impoverished, with diseases of abuse and neglect,” he remembers. “I felt passionately that to those who much is given, much is expected.”
That’s a perspective shared by Keeshin, whom Spivak brought into the conversation with Madsen. Keeshin was adopted as an orphan in Bolivia and raised by a family in Utah. “I felt like I was given so many opportunities in my life,” she says, “adopted to a family that had the means to get me educated.”
Growing up in Utah, HIV first made its mark on Keeshin’s life as a teenager at Skyline High School, when gay friends shared their fears about the future. “One said, ‘I’m going to get HIV and die, and probably half of us will,” she recalls.
Keeshin applied to Meharry Medical College, a historically black institution in Nashville, Tenn., to study medicine, drawn in part by the school’s philosophy of serving the under-served. “It’s more of an emotional relationship than I think traditional medicine is,” she says. “Just seeing the interaction of patients and HIV doctors, it’s so close. You share their highs and lows, go to their birthday parties. You’re part of each other’s lives. They’re not just a diagnosis.”
The level of demand for PrEP had opened Spivak’s eyes. At University of Utah Hospital’s Infectious Disease Clinic, where both he and Keeshin work, about 100 people—all insured white men—are on PrEP, Spivak says. Many uninsured people had gone to UAF for PrEP and been told there wasn’t a way for them to access the drug yet. “These are people who sought out UAF [and] think they’re at risk of HIV,” Spivak says. “Everyone I talk to who thinks that, they’re right. Patients know they want this and they can’t get it. What is the barrier? Gilead [the manufacturer] gives patients the drug for free. The barrier is the system.”
In fact, UAF believes that far more people want PrEP than their numbers indicate: “Uninsured people might not seek services believing they are out of financial reach,” Herrschaft writes in an email.

Susan Keeshin Credit: Jen Pilgreen
COMING DOWN FROM THE HILL
In October 2017, Spivak and Keeshin met with Kathleen A. Cooney, then the chair of internal medicine, and showed her data from UAF that demonstrated the unmet need for PrEP in Salt Lake Valley. They told her that only people who had insurance could get PrEP, but they knew people in the city who wanted it and couldn’t get it. Spivak offered a tantalizing proposition: Would you like to stamp out HIV in your own backyard?
Cooney gave them a seed grant from her discretionary chair funds to start the clinic. “Then we just relied on our friends,” Keeshin says. The nurse manager at the infectious disease clinic volunteered her time. ARUP provided a manageable price on laboratory tests. A volunteer case manager helped clients access PrEP free via Gilead’s patient assistance program. Communications and IT helped build a website to get the word out. “We asked a lot of people, ‘Hey, can you help us with this?’” Keeshin notes. “And it all came together.”
Madsen and Weis worked hard to spread the word about the clinic and attract volunteers among U of U Health’s student body. Madsen organized a training day in late 2017 where 120 first- and second-year students took mock sexual histories from LGBTQ patients. “It can be uncomfortable to sit down with a doctor and use big terms,” he says. Rather than desexualize activity by making it scientific, he and other clinic staffers use gay vernacular found on dating apps.
The clinic leadership secured free space at Redwood Health Center on 2100 South, east of Redwood Road. The location was crucial: They wanted somewhere neutral, out of the way, and discreet.
“We’ve engineered this clinic to try to align it to the patient population we want to treat, as opposed to the standard model of health care,” Spivak says. Its location near West Valley City places the clinic close to many uninsured patients; for those without access to transportation, a TRAX station is nearby. “We wanted to make it a point that we were in the community,” Spivak says. “We wanted to be an equal.”
SO MUCH MORE THAN AN HIV STATUS
The clinic leadership announced their plans to the gay community at a World AIDS Day event on Dec. 1, 2017 at Ember, a downtown Salt Lake City venue. With help from U of U Health, UAF and other community supporters organized food and decorations, as well as a candlelit vigil at the Salt Lake City and County Building, which was bathed in red light to mark this seminal day of awareness and remembrance. A crowd of nearly 40 people held a moment of silence to remember those lost to HIV and AIDS, candlelight flickering over their faces.
Spivak remembered a young woman and talented artist who had acquired HIV from her ex-husband, who was both abusive and, unbeknownst to her, an IV drug user. She’d gone to the hospital delirious and burning up; two hours later, she was diagnosed with HIV/AIDS and lymphoma. She died two years later.
Keeshin recalled a transwoman patient who had been murdered.
Madsen thought about how lucky he was to have been born after the AIDS crisis, even as its ripples continue to wash up on his life every day. He thought about an old college friend, a drug-using gay man who struggled so much with his HIV status, his sexuality, and his addiction that he took his own life. “For me, he is a testament that no patient is ever just a disease but a complex human being,” Madsen writes in an email. “His life was so much more than his HIV status—but that status also impacted every single aspect of his life.”
Weis was out of the country at that time, working at a hospital in Rwanda with local doctors treating patients with HIV infections. She saw in horrific, painful detail the price patients paid for the failure to prevent and diagnose HIV infections. “These are people who should have had a fair shake in life, but they were dying,” she says. When she returned to Utah in February 2018, she knew unequivocally that “preventive health care is the way we are going to stop the epidemic in the U.S.” She told Madsen, “I want to be right there with you. I’m in.”

Adam Spivak Credit: Jen Pilgreen
OPENING DAY
After building a career in academic medical centers and the massive, bureaucratic machinery of medical research, Spivak found himself in the midst of creating something new. Then, one Saturday morning in March 2018, the first patient entered a room. He had to remind himself to not overwhelm the man with his excitement and enthusiasm. “Don’t get too effusive,” Spivak told himself. “It’s not about you.” Nevertheless, after the first patient came out, the staff cheered.
As exciting as opening day was, it also presented a steep learning curve. “A patient comes, then what?” Keeshin says. “That was a little awkward.” She became a traffic controller of sorts, working with Weis to streamline the patient’s intake, first talking to an assistant, then a doctor, and then a case manager to get their paperwork in to Gilead to apply for financial assistance, a three- to four-week process.
One patient who attended the clinic when it first opened was “Carlos,” referred by UAF after he went to the nonprofit for an HIV screening. The 39-year-old had thought he couldn’t afford PrEP. Now that he’s on the drug, he says, “I feel more safe when I meet somebody.”
Weis expected the clinic to “limp along” in its first year, with patient counts barely breaking into double figures. As the months went by, the five to 10 new patients arriving in the first weeks quickly increased until they had more than 100 patients on their books. “Clearly, their client load is suggesting there’s even more need than they anticipated,” UAF’s Executive Director Stan Penfold says.
Patients routinely expressed their gratitude to Spivak for the non-judgmental environment of the clinic, something that he was puzzled about when Madsen had first brought it up. Madsen insisted that the clinic should be LGBTQ-friendly, with staff expected to understand the gay vernacular, but Spivak was surprised at what he felt was obvious: “Of course we’re going to be LGBTQ-friendly,” he thought. Now he understood Madsen’s concerns. “Patients would share really awful experiences in 2018 in Utah,” Spivak says, “of going to physicians’ offices, being singled out, being told to leave, being told ‘we don’t provide that service here,’ ‘we’re not seeing you,’ just really awful stuff where folks are seeking out help and it’s not there for them. I wasn’t aware that this stigma was that extensive, and I’m an HIV doc. I should know that.”
Every other Saturday, Weis sees couples dealing with what she calls “leaps of faith,” where one partner takes PrEP so they can stay with someone who is HIV positive. “We decided to get tested together; he came up positive, I came up negative,” is the story she often hears.
One Saturday morning saw several return patients, including a couple: one on PrEP, the other positive. “They were very loving,” Weis says. “It was really beautiful to watch them with each other.” They had just learned that the positive man’s viral load had been suppressed through medication. He was undetectable, meaning that the virus was essentially untransmissable. That’s the ultimate goal, she says: to get an HIV positive person’s viral load so low it’s undetectable, with the negative person they are having sex with on PrEP.

Juan Marquez Credit: Jen Pilgreen
AMBASSADORS FOR PrEP
On a mid-October Saturday morning, Spivak stands in the PrEP clinic’s hallway and glances at the consulting rooms. All the doors are closed. At the Infectious Disease Clinic, which Spivak calls “a well-oiled machine,” 20 to 30 percent of their appointments are no-shows. At the PrEP clinic, it’s about 10 percent.
At a clinic that didn’t advertise until a few weeks before via a free ad on Grindr, every room is full. That’s the first time that’s happened, he says. “Word is out I guess.”
Among those who transmitted that word are passionate patient-advocates for PrEP. “Patients were taking pictures of our business cards and putting them on dating apps,” Madsen says. One such advocate is court interpreter Juan Marquez, who Keeshin calls “my PrEP champion.” She adds, “He’s taken it upon himself to put the word out in the Latino community.”
Marquez’s introduction to PrEP came while filling out paperwork in a doctor’s office, where a nurse told him about the medication. “It seemed too good to be true,” he says. When he went to see Keeshin for the first time—he has insurance through his job—she told him that taking PrEP was an act of responsibility.
After Keeshin told him about the PrEP clinic, Marquez offered information about free PrEP on on his Grindr profile for anyone that wanted it. He also posted similar offers on Facebook. “I make sure to say it’s not a gay pill,” he says. “It’s for you if you’re not infected.” He’s had more than 100 people ask for information.
On one visit to the clinic, Keeshin asked him, “Did you ever post on this on Grindr? I think some of my patients are your referrals.” Several patients had talked about Marquez’s advocacy efforts through social media, and she’d recognized him from their description of his profile picture on Grindr.
That was Marquez’s ah-ha moment. “Wow, people care,” he thought.
PROUD TO BE UTAHN, PROUD TO BE GAY
On Nov. 29, 2018, the clinic and the Utah Aids Foundation hosted its second World AIDS Day fundraiser, Red Party, hosted by Tan France, the star of Netflix’s Queer Eye reboot. “We’re looking to expand,” Madsen says. “We have an overwhelming need in the community for PrEP.”
Beyond the fundraiser, Spivak and Keeshin hope to raise $500,000. That would allow them to open every Saturday morning instead of every other one, and also purchase a van to use as a mobile clinic so they can do outreach to addicts, the homeless, street sex workers and other high-risk populations.

2018 Red Party HIV fundraiser
In October and November, Madsen and Weis interviewed for residency positions at high-profile out-of-state hospitals. Before Madsen co-founded the clinic, he wanted to leave Utah as fast as he could. Now, it’s hard to depart. “This is like my baby,” he says. “I don’t want to hand it off. [The clinic has] given me confidence. It’s given me a sense of purpose. It’s made me very proud to be a gay man.”
Marquez has also found his self-assigned work as a clinic advocate rewarding. A young man he’d told about the clinic reached out for information months later. He works part-time work and goes to college thanks to DACA while supporting his single mother. PrEP was a luxury he couldn’t afford, he told Marquez, who responded that the clinic was free.
A few weeks later, he got a text with a photograph of a prescription labeled bottle of PrEP. “Look what I just got!!!!” his friend texted, with a smiling emoji. “I’m so excited.”
“Omg!!!!!!!!!!!” Marquez texted back. “I’m so excited for you.”
“Yass. I’m starting tomorrow.”
Spivak spells out just how high the stakes are for Utah and for those at risk of infection. “The only state ever in the country to drive down HIV rates? It’s never happened,” he says. “We. Can. Do. That. We are doing that. We have the opportunity in this small, tight community to stamp all this out. We can end the spread of HIV in Utah.”
Banner image of Jorgen Madsen at the PrEP clinic. Photo credit: Jen Pilgreen

